Post A Comment
Cancel Reply
This site uses Akismet to reduce spam. Learn how your comment data is processed.
This edition of Apollo Knows is all about an ACL tear.
Specifically, the purpose of this write up is dedicated to educating high school and college athletes, weekend warriors, the general population and anyone else who has suffered an ACL tear.
When you are finished reading, I hope you feel more empowered to take your ACL tear rehab head on.
The most common mechanism of an ACL tear occurs when an individual’s knee is fully extended or bent inwards while:
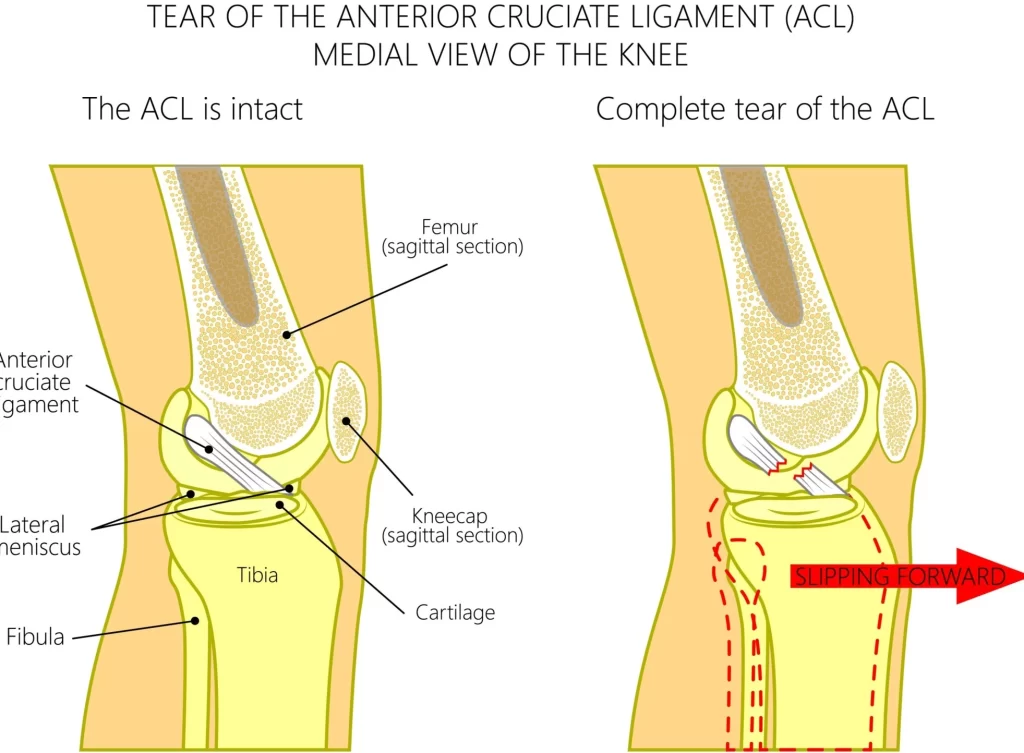
During these scenarios, it is thought the quadriceps are over-activated, while the hamstrings are under-activated. This doesn’t mean you necessarily have weak hamstrings, it just means that the way your body is positioned is telling your quadriceps to fire rapidly in attempt to protect yourself. Consequently, the quadriceps pulls the tibia forward, and can result in an ACL tear.
As you can probably assume from reading above or watching sports, the majority of ACL injuries are “non-contact” injuries.
That is, they often don’t occur during a collision, such as getting tackled in football (although still possible). Matter of fact, 70% of ACL injuries are non-contact injuries [1]!
As much as I would like to say you should seek out Phyiscal Therapy first, I believe it is best to receive an MRI as soon as you can.
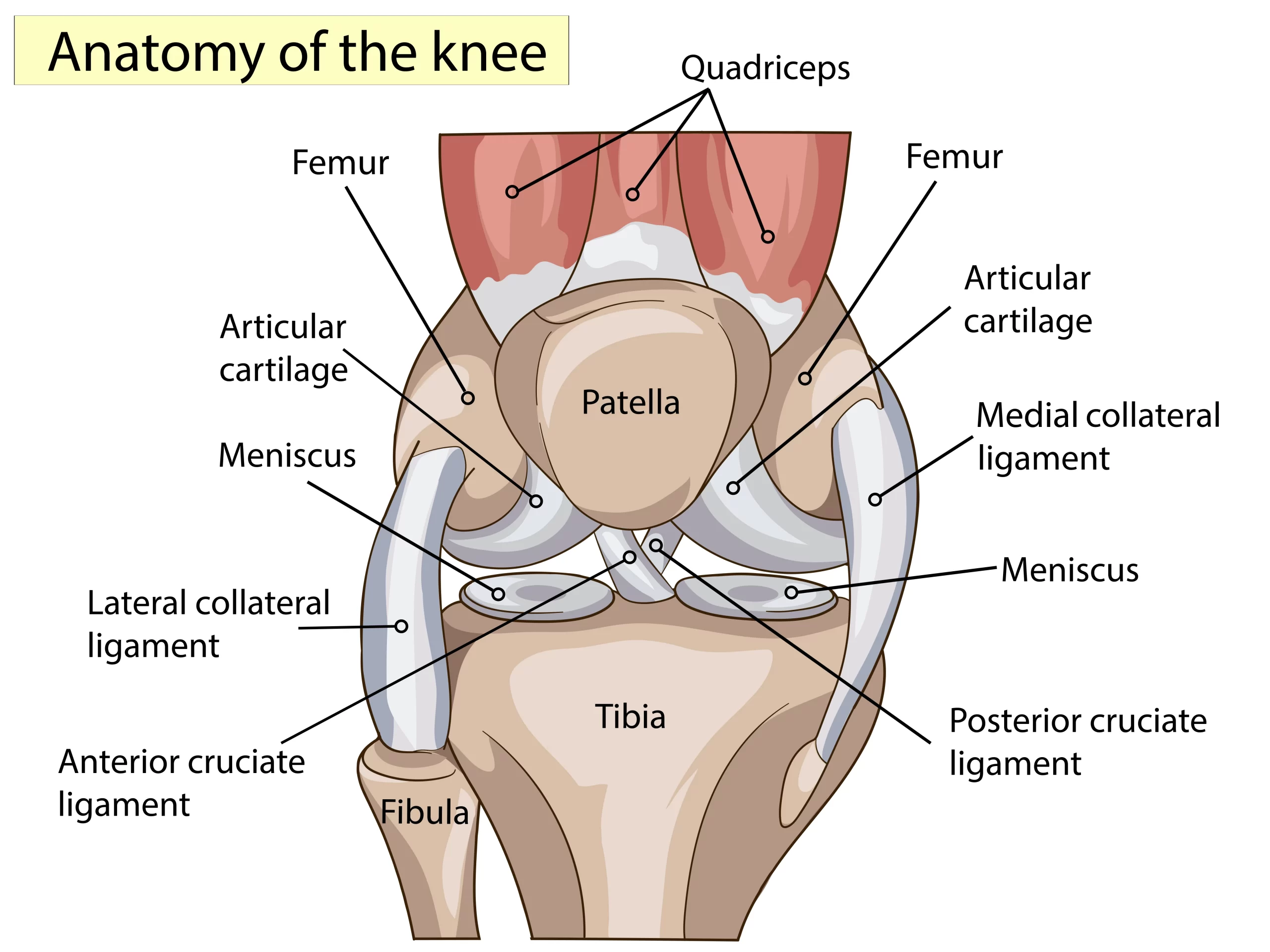
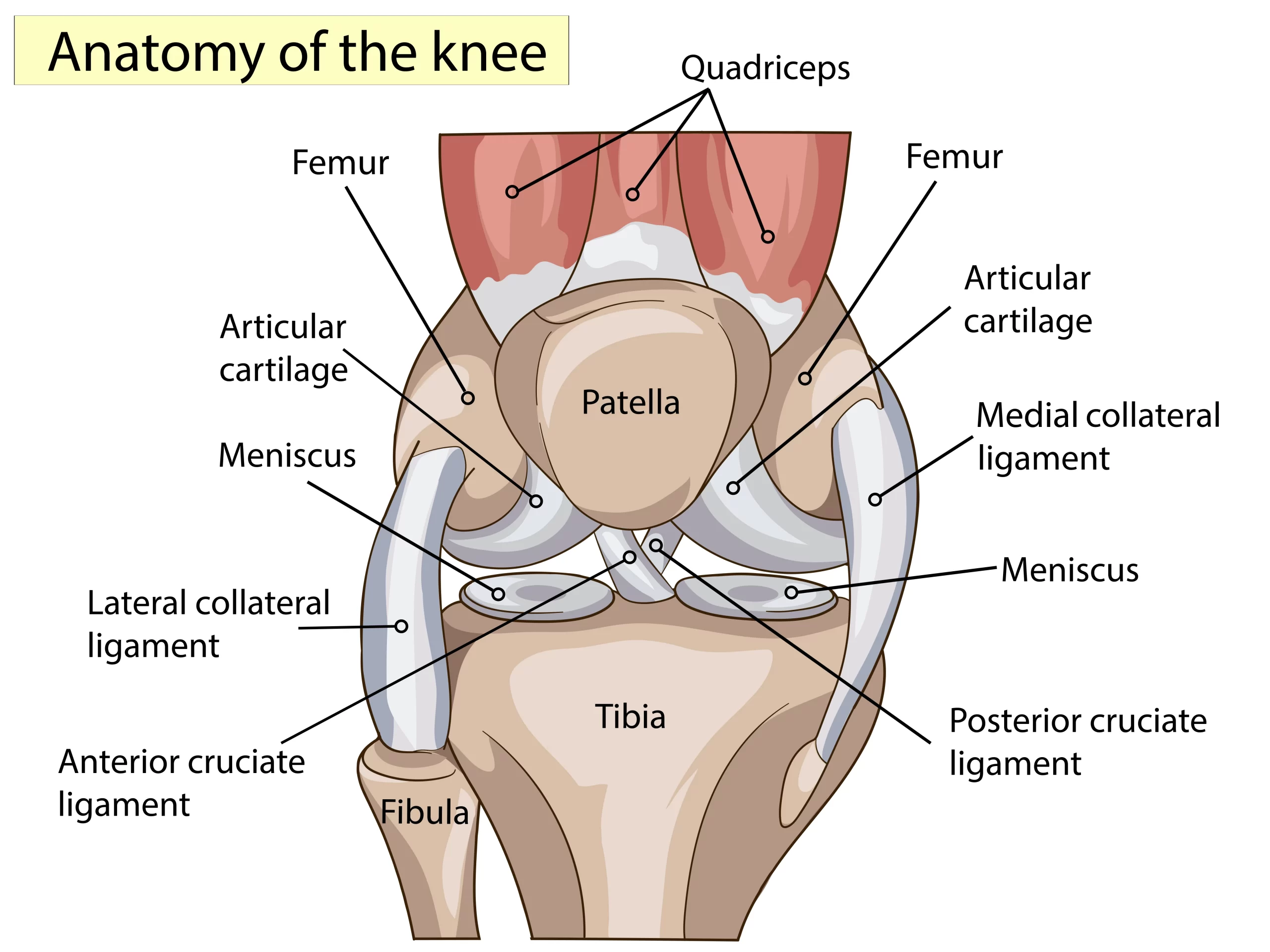
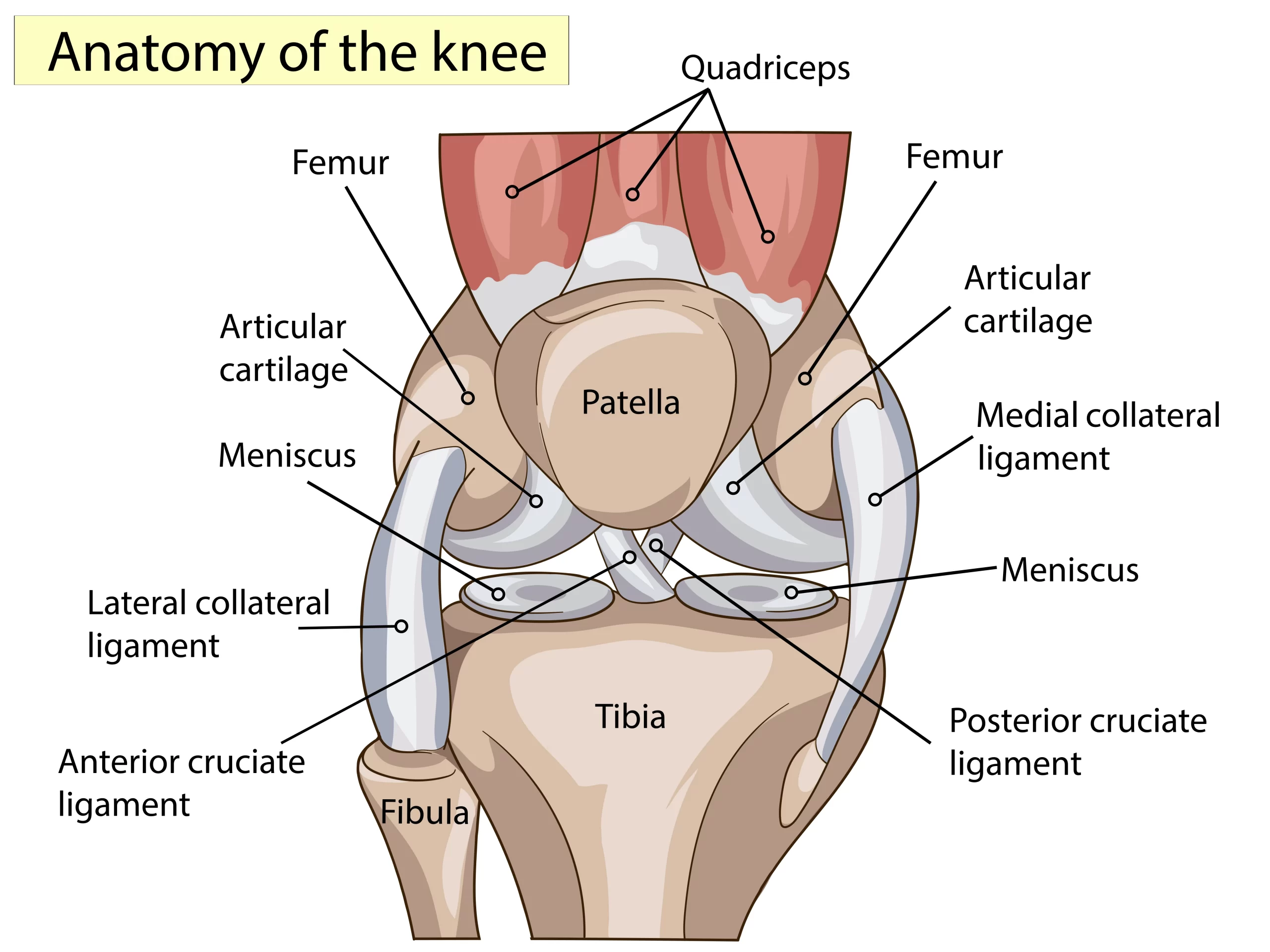
An MRI can be helpful in providing you with an accurate diagnosis and prognosis by identifying the complexity of your injury. Other injuries have found to occur with an ACL injury, such as [2]:
Knowing if other tissues were damaged is valuable in not only determining how long it will take to recover, but also to guide rehab.
For example, if there is an MCL injury as well, movement in certain directions will be limited for a period of time.
Furthermore, if a meniscus injury is present, there will be an extended period of not putting any weight on your leg.
As already mentioned, the MRI is the gold standard in diagnosing an ACL tear as well as for other injuries that may have occurred at the same time.
You may wonder, can a Physical Therapist perform testing to tell if you have an ACL tear?
The answer is YES.
Physical Therapists can perform a test called the Lachman test to assess for the presence of a torn ACL. The Lachman test has been found to have similar accuracy to an MRI [2].
I just recommend getting an MRI first, as the MRI is more accurate in picking up the additional injuries that may have occurred.

It’s hard to imagine not needing surgery for such a gruesome injury.
That being said, when compared to surgery, there are individuals who have had comparable results with Physical Therapy alone!
When a complete ACL tear occurs it can be thought of as a bomb going off that completely destroys the ACL into small chunks.
Thus, the ACL cannot just simply be reattached. So, new tissue needs to be used to form a new ACL. That is where the name of the surgery, ACL reconstruction, comes from as the ACL has to be completely rebuilt with new tissue.
That being said, new research is aiming to figure out if a ruptured ACL can spontaneously heal.
The two most common approaches to ACL reconstruction deal with using either a patella tendon graft or a hamstring graft.
A graft refers to the process of using tissue from one area of the body to repair injured tissue in a different area of the body.
When a patella tendon graft is used, the central 1/3rd of the patella tendon is removed to replace the torn ACL.
A hamstring graft is used in a similar matter. When a hamstring graft is used, a portion of your semitendinosus (one of your hamstring muscles) is cut out and used to replace the torn ACL.
In summary, Physical Therapists are not surgeons!
For more detailed information regarding the surgical process for an ACL tear, I recommended reading the write up done by the American Academy of Orthopedic Surgeons.
The ACL rehab process is not something that should be taken lightly.
The financial burden, psychological distress, and physical impairment that an ACL tear brings upon a person warrants a thorough, detailed rehabilitation process.
This section of this blog is dedicated to how your Physical Therapist can help with an ACL tear BEFORE SURGERY OR WITHOUT SURGERY to achieve the best possible outcome.
If you can tell from this blog post, Physical Therapists do have some knowledge on surgical process. Thus, along with a surgeon, your Physical Therapist can help you decide on which of the 3 treatment options for ACL tears is best for you when deciding on surgery.
The surgical procedure generally will be less than 2 hours, from which you will wake up feeling groggy. In order to reduce pain upon awakening from surgery, a nerve block is used by some surgeons. Generally, a nerve block will last the first few days after surgery.
It will be challenging to move your leg after surgery. A downside of a nerve block is the challenges it can pose on moving your leg initially. A nerve block will cause your leg to go numb and thus, will make it extremely difficult to move your leg at all.
Furthermore, inflammation that forms around the knee after surgery will make moving your leg even more difficult.
The inflammation will block nerve signals that are sent to your muscles, specifically the quadriceps, and prevent them from working in their usual ways.
Don’t worry though!
Although altered sensations may be experienced for weeks, you should be able to move your leg within a couple days.
Once your surgeon, nurse, or physician assistant ensures your pain levels are stable, you will be discharged! This is almost always the same day of the surgery.
There are several assessments that Physical Therapists can perform to give you a prognosis on the severity of your injury and expectations for your outcomes.
Setting goals on day 1 will guide the entire rehab process!
If your Physical Therapist is not asking about your goals on day 1, find a new Physical Therapist.
Once your goals are set, your Physical Therapist can assist with making a plan to achieve your goals and provide a realistic time frame to achieve those goals.
There are specific “benchmarks” that have shown to improve outcomes in the long run if they are achieved before surgery. Some of these benchmarks include [8]:
Athletes undergoing a 5 week period of rehab before having surgery have found to return to sports sooner as well has report higher function compared to individuals not electing for a period of Physical Therapy prior to surgery. This 5 week program involves improving strength and neuromuscular function [8] [9] [10]
Addressing fear is something that needs to be re-evaluated and addressed throughout the rehab process.
When it comes time to return to sport, athletes state fear is a bigger concern than problems with their actually knee itself [2].
Your Physical Therapist can work with you to improve your confidence by using strategies such as goal setting, motivational interviewing, or cognitive behavioral strategies.
There comes a time where the rehab process WITHOUT surgery is no different than it is WITH surgery.
Read below on how Physical Therapists can help increase your knee motion, strength, balance, and getting you ready to return back to playing your sport
Along with providing a prognosis, assisting with setting goals, and addressing fear, as is done with or without ACL surgery, Physical Therapists also have a lot to offer AFTER surgery.
This section of this blog is dedicated to how your Physical Therapist can help you out AFTER SURGERY to achieve the best possible outcome.
Depending on the type of graft used there are certain precautions that need to be taken to ensure optimal outcomes.
For example, a hamstring graft needs a period of avoiding stretching to protect the tissue. Everyday tasks, such as bending down to tie your shoes will stretch the hamstring and should be avoided for a period of time.
Your Physical Therapist should guide you on proper ways to decrease swelling as early as possible after surgery. When swelling persists it can have a cascade affect in your ability to recover.
For example, achieving full range of motion is vital early on and this may be challenging if swelling persists
Increasing your ability to bend your knee is something that should be addressed early by your Physcial Therapist to not only improve movement, but also to:
Your Physical Therapist should also assess your motion in your ankle and hip as well. Similar to deficits in knee motion, decreased motion in the ankle and hip can alter the stress going through your knee.
For example, decreased ankle range of motion can limit your ability to bend your knees while squatting. In order to compensate for decreased ankle motion, you will likely squat with your heels off the ground, which will increase the stress going through your knees!
Strengthening is one of the core components of a rehabilitation program for ACL tears. A good Physical Therapist will emphasize the importance of strengthening your entire body, not just the muscles that are near your knee.
For example, hip weakness has been identified as a possible risk factor for suffering an ACL tear [11]. As such, exercises that strengthen the hip musculature is vital for proper recovery.
The exercise progression usually begins very basic (ie straight leg raises), but evenutally you should be doing deadlifts, etc depending on your goals.
How ACL rehab will start:

How ACL rehab SHOULD progress:

A common term that you will hear Physical Therapists say a lot is “neuromuscular training.”
This is really just a fancy term for working on strengthening the connections between your brain (“neuro”) and your muscles (“muscular”) in order to move more efficiently and under control “”training.”
Nevertheless, neuromuscular training or balance training is absolutely critical to ACL tear rehab.
Your ACL has mechanoreceptors, which are nerve receptors that tell our brain where our knee is in space [12].
So, when the ACL ruptures, these connections get disrupted and it can be challenging to move again. Luckily, research has shown that interventions that target neuromuscular control can improve this deficit.
Interventions that your Physical Therapist may use to improve your neuromuscular control include:
This is usually the most exciting phase of rehabbing from an ACL tear. This can also be the most challenging phase mentally.
Often times, the athlete will feel like they can start playing their sport again sooer than they should.
This can be a hard concept to understand, but emerging evidence states the actual graft itself takes around 9 months to heal [13].
That is, even though you feel stronger, are running again, etc your graft still may need time to properly heal to avoid re-tearing your ACL.
To further emphasize the importance of allowing the graft to heal, I want to break down what I mean by “heal.” An ACL graft does not heal like a scab on your knee heals.
Your ACL graft is heals by becoming adjusted to your body. In other words, an ACL graft requires load to be placed on it so that it can adapt to your activities. Remember, an ACL graft is a tendon, NOT a ligament.
However, it is thought to be important to get the ACL graft to function like a ligament. It is thought that the ACL graft requires load over an extended period of time in order to start behaving like a ligament.
For the purpose of this write up, I broke the return to sport training phase into 3 parts:
Starting to run again after recovering from an ACL tear is a huge milestone, but it’s important that this phase is implemented correctly.
Your Physical Therapist should provide interventions and continually reassess till these criteria are met before you begin running:

Beginning to run again should also be introduced gradually to ensure proper running form is used and to get your muscles, tendons, and ligaments used to to running again.
Your Physical Therapist can work with you to design a running program that starts at a slow speed and short distance and gradually increase the difficulty.
In the end stages of rehab, your running program may include a variety of different speeds and distances. The purpose of this is to allow our muscles to get used to different types of loads.
Our muscles are adaptable to the loads placed on them, so it is important to place a variety of loads on our muscles to ensure they are ready for all kinds of sports or activities.
For example, if you only run at your “comfortable jogging speed”, your tissues will only be used to the load that occurs with that speed. Consequently, if you were to ever have to sprint, your tissues would not be used to that type of load since you never practiced it.
Similar to beginning to run again, beginning to jump again is another huge accomplishment for athletes. But, if done improperly, this can lead to more issues. Your Physical Therapist can work with you to ensure you have proper form to protect the ACL from future injuries.
Some common interventions that are used during this phase include:
This part of the rehab process should be very individualized to the athlete’s sport. Although not necessary, it can be helpful if the Physical Therapist is familiar with the sport so they have a better understanding of the movement patterns involved with the athlete’s sport.
Interventions in this phase vary by sport, but here are some examples:
There are numerous assessments your Physical Therapist can perform to evaluate if you are ready to get back to playing your sport.
There are specific criteria that each test has that must be achieved in order to get back to playing your sport. The research has shown that achieving these criteria can decrease your chance of re-injuring your ACL.
Common return to sport testing involves:
A single ACL surgery has been found to cost $38,000 [15], so you can imagine the importance of proper rehabilitation.
There are several evidence based prevention programs in place, such as the PEP [16], that has shown to prevent injuries in sports.
In my opinion, the best strategy to prevent a re-tear or an ACL tear in the first place is staying in shape year round.
That means continued lifting, conditioning, balancing, and jumping exercises. Just because you meet the “return to sport criteria” does not mean that you are healthy for the rest of your life, it just means your are healthy at that time point.
For example, once you achieve the quadriceps strength criteria does not mean your quad will stay that strong forever. If you don’t continue strengthening it, it will decrease and then you are right back in the risky territory of suffering an ACL tear.
Annual or biannual visits with a Physical Therapist could be beneficial in reassessing the “return to sport” criteria to ensure you are maintaining tip top shape.
Your Physical Therapist and Surgeon both bring something to the table in making this decision. In a perfect world, your Physical Therapist and Surgeon BOTH agree that it is safe to return to playing your sport.
Where it gets tricky is when your surgeon clears you, but your Physical Therapist hasn’t, or vice versa. Which unfortunately, can happen.
If that is your case, consider these thoughts:
If this is your case, read our blog to learn more about who should clear you to return to sports.
This site uses Akismet to reduce spam. Learn how your comment data is processed.

No Comments