
Complete Guide For Patellofemoral Pain Syndrome Rehab

2 Comments
Post A Comment
Cancel Reply
This site uses Akismet to reduce spam. Learn how your comment data is processed.

If you are a basketball player, soccer player, recreational runner, in the military, or just enjoy binge watching Netflix, this article is for you.
If you are a teen or adult, women or man, tall or short, or obese or fit, this article is for you too.
Essentially, this article is for EVERYONE looking to learn about Patellofemoral Pain Syndrome rehab.
Patellofemoral Pain Syndrome has become one of the most common, yet misunderstood conditions involving the knee. It has been found to affect essentially every individual regardless of age, gender, height, or BMI.
Not only does this condition affect all kinds of individuals, the symptoms that individuals experience vary from person to person.
Furthermore, individuals often respond differently to Patellofemoral Pain Syndrome rehab. For example, two different people performing the same treatment may respond differently.
Due to the varied presentation and challenges with treating this condition, it is beginning to be described as the “low back pain” of the knee.
On the bright side, Patellofemoral Pain Syndrome rehab has shown to:
By reading this edition of Apollo Knows, you will learn the following about Patellofemoral Pain Syndrome:
Patellofemoral Pain Syndrome is not as easily described compared to other conditions or injuries. This is because it is considered a “diagnosis of exclusion” [1].
A diagnosis of exclusion refers to a diagnosis given after ALL other possible diagnoses have been ruled out. And if you didn’t already know, this requires a lot of other possible injuries to be ruled out.
The most simple way to define this condition is by describing the most common symptom, which is anterior knee pain.
Some healthcare professionals have even started to call this condition “anterior knee pain.” However, this condition is still commonly referred to as “Patellofemoral Pain Syndrome.”
More specifically, this condition describes pain in the patellofemoral joint (knee joint) that often occurs from unknown causes, but presents with similar symptoms hence “syndrome.”
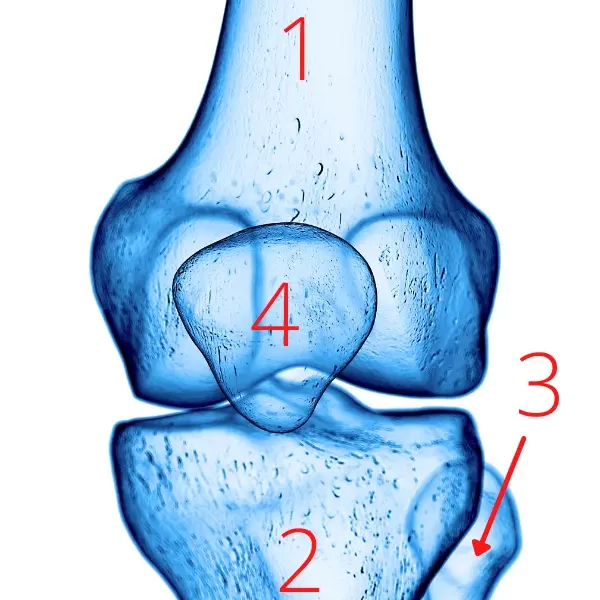
The patellofemoral joint is used to describe one of the joints that make up the knee joint. The bones that compose the knee joint include:
Like I already said, A LOT of other diagnoses must be ruled out when diagnosing Patellofemoral Pain Syndrome. That is because of all the nearby structures.
The structures that are in close approximately to the patellofemoral joint include:
Due to the difficulty in diagnosing this condition, identifying factors that may put one at risk for developing Patellofemoral Pain Syndrome is challenging.
Furthermore, research that is continuing to emerge is contradicting the findings from previous research on the risk factors for developing Patellofemoral Pain Syndrome.
If you have had Patellofemoral Pain Syndrome rehab in the past, take a look at the list of risk factors below. If you were told about various factors that played a role in developing Patellofemoral Pain Syndrome, you would be told something different today.
What were once thought to be risk factors [2] [3] [4]:
What the current evidence says [1] [5]:

Notice any differences between what was once previously thought to be risk factors compared to the latest evidence?
If you don’t, then you need to start wearing some gla… ah nevermind, you’ll figure it out eventually.
The differences between the two lists are massive!
The first thing that I notice is the addition of all the “maybe’s” under the current evidence list. This can be explained by the most recent evidence demonstrating different findings from past studies.
Are you a little confused? Me too.
It doesn’t make a lot of sense how so many risk factors can all of a sudden be considered questionable! Furthermore, it doesn’t make sense how hip weakness AND increased hip strength are on the list. This just goes to show we clearly need even more research to learn more.
The next thing that I observed was that the current evidence list is full of risk factors that can be addressed during Patellofemoral Pain Syndrome rehab. This is a good thing!
I also noticed that although there are less risk factors in the current evidence list, there are still a lot. This goes to show how complex this condition is!
The final observation I made was the addition of psychological factors onto the current evidence list.
Are you confused on this one too? Check out my blog post on mental health and Patellofemoral Pain Syndrome.
If you google, “What causes Patellofemoral Pain Syndrome”, it will likely say something about overusing or overloading the patellofemoral joint.
This is afterall the most common cause that is reported in recent studies [1] [6].
Many athletes experience this condition at some point. Failing to train for an upcoming season can lead to overuse injuries. As Patellofemoral Pain Syndrome is considered an overuse injury, this is where the overuse/overload cause of this condition stems from.

Although overuse leading to Patellofemoral Pain Syndrome in athletes is common, it can occur in any active individual. Specifically, excessive running and squatting movements have been linked to this condition.
I wish I could stop typing and move on, but that would be doing you a disservice.
Unfortunately, the cause of Patellofemoral Pain Syndrome is not as simple as simply attributing overuse as the single cause.
Patellofemoral Pain Syndrome is common in more than just athletes and active individuals. It is also seen in sedentary individuals that don’t exercise at all and work a desk job 8 hours a day.
Are you going to say their Patellofemoral Pain Syndrome is from overuse too?
Most people present to Physical Therapy saying something like, “My knee hurts when sitting for a long time and when going up and down stairs, but I don’t know what I did to hurt myself.”
They don’t describe changing directions suddenly and instantly feeling pain. Nor will they recall a traumatic event, such as a collision in soccer. They just state, “I don’t know what I did.”
Of course, there are times when patients say something similar and a Physical Therapist can eventually identify the cause of an injury. Patellofemoral Pain Syndrome is often not one of those scenarios, however.
Due to the challenge in identifying a specific event and the long list of risk factors, the cause of Patellofemoral Pain Syndrome is often considered multifactorial [1] [7]. That is, this condition is thought to occur from several factors.
If you ever require Patellofemoral Pain Syndrome rehab, your Physical Therapist will know the cause of this condition is multifactorial. As such, they will likely explain what caused your injury using multiple reasons (multifactorial) such as:
“Your hip and quad muscles are weak”
“Your gluteus medius and core are not strong enough to stabilize your leg”
“Your VMO is delayed and your quads are tight”
“Your glutes are weak and you have altered patella tracking”
“Your patella is not tracking correctly”
Although these responses may seem appropriate, there is an issue with them.
I’ll illustrate this issue with an example.
Let’s say you go to a Physical Therapist and they say that you have Patellofemoral Pain Syndrome.
Your Physical Therapist then explains that your Patellofemoral Pain Syndrome occurred due to delayed VMO activation. For the purpose of the example, we will assume your Physical Therapist is very good and you in fact do have delayed VMO activation.
You would then likely nod your head yes, while wondering what in the world VMO is.
But, have you ever thought that it is possible that you have had delayed VMO activation for years?
Unless you frequently check your VMO activation yourself, you wouldn’t know. And unless your besties with your Physical Therapist, they FOR SURE would not know either!
So if it’s impossible to say when your delayed VMO activation started, then it’s not accurate to say it caused your Patellofemoral Pain Syndrome.
Furthermore, all of the examples I mentioned above are RISK FACTORS that have been associated with developing Patellofemoral Pain Syndrome at some point in time. They are NOT used to describe what causes this condition.
In my opinion, saying the cause of Patellofemoral Pain Syndrome is multifactorial is really a big fancy word for saying we don’t really know what the cause is.
I’m telling you this not to scare you, but to inform you. I don’t want your Physical Therapist, Physician Assistant, or anyone else to trick you into thinking they know why you have this condition, when in reality, they don’t. Nobody does.
Even though the cause of this condition is not understood, the benefits that Patellofemoral Pain Syndrome rehab can have is understood.
For that reason, I usually tell people that appear to have Patellofemoral Pain Syndrome something like, “It’s not really known what causes this. What is known is how Patellofemoral Pain Syndrome rehab can help you back to living your life with less pain.”
So in summary, If you did end up asking Google, “What causes Patellofemoral Pain Syndrome”, somewhere in Google’s answer should also include something like “unknown” or “multifactorial.” If it doesn’t, Google is wrong.
For how misunderstood Patellofemoral Pain Syndrome is, the symptoms of this condition are more agreed upon.
Other symptoms include:
These symptoms appear to be straightforward, however, individuals with Patellofemoral Pain Syndrome often experience different symptoms.
For example, one person may only feel pain while sitting, while another person may only feel pain while squatting.
Furthermore, MANY different injuries cause anterior knee pain. This is why the first step of Patellofemoral Pain Syndrome rehab is ruling out other possible injuries.
Before I say anything, let me preface by saying it doesn’t matter what I say, your medical doctor says, or anyone else in regard to what medical professional you should see first.
The only thing that matters is what YOU want to do.
If you feel more comfortable with going to an orthopedic doctor, go for it. If you go to your primary medical doctor for everything, there is nothing wrong with seeing them first either.
However, with deductibles increasing dramatically year after year, receiving medical care is becoming more expensive. If you are worried about how much it will cost to figure out you or your kids’ knee pain, then you may want to listen to what I have to say.
No matter what medical professional you decide to see first, they SHOULD be referring you to Physical Therapy right away.

Patellofemoral Pain Syndrome rehab with a Physical Therapist is the first line of defense when treating this condition. I PROMISE that I am not making that up. I am saying that because that is what the most recent evidence states [7] [8] [9].
Patellofemoral Pain Syndrome rehab is the first line of defense due to the following [8]:
If the above is true, doesn’t it make sense to begin Patellofemoral Pain Syndrome rehab with a Physical Therapist first?
It makes even more sense due to the fact that Patellofemoral Pain Syndrome rehab with a Physical Therapist has shown to [1] [7] [10] [11] [12] [13] [14]:
Furthermore, if any imaging is needed, Physical Therapists are educated on the presence of signs and symptoms that would require imaging.
I realize that some insurances require a prescription to attend Physical Therapy. But, if your insurance does not require a prescription, beginning Patellofemoral Pain Syndrome rehab with a Physical Therapist can save you lots of money.
Remember, Patellofemoral Pain Syndrome is a diagnosis of exclusion. This means that EVERY POSSIBLE INJURY must be ruled out before beginning Patellofemoral Pain Syndrome rehab.
Other injuries can be ruled out primarily by taking into account your symptoms and cause of injury.
Another way that your Physical Therapist will rule out other injuries is by performing “special tests.” Special tests are specific movements that aim to reproduce your symptoms or assess the presence of impairments that are consistent with other injuries.
There are essentially special tests for every kind of injury, including Patellofemoral Pain Syndrome.
Some of the special tests for Patellofemoral Pain Syndrome that your Physical Therapist may perform include:
However, the ability of special tests to diagnose Patellofemoral Pain Syndrome are not supported by strong evidence [1]. As such, your Physical Therapist will attempt to reproduce your symptoms in other ways.
Your Physical Therapist will attempt to reproduce your anterior knee pain by having your perform the following:
In summary, due to the poor ability of special tests to diagnose Patellofemoral Pain Syndrome, the diagnosis is based on two criteria [1]:
There was a study that compared two treatment options for those with chronic Patellofemoral Pain Syndrome. The two treatment options were [15]:
What treatment option would you pick?
Stop reading.
Don’t scroll down till you answer.
Well, it doesn’t really matter what treatment option that you would pick!
Both treatment options were found to have similar outcomes up to 5 years later [15].
As much as I would like to hold a cardboard sign on a random corner saying “Surgery Sucks”, I won’t. I wouldn’t feel confident in making a bold statement based on one study.
Why don’t I just read more studies?
Unfortunately, surgery and Physical Therapy have not been compared much more.
As such, Patellofemoral Pain Syndrome rehab is advised to be used initially rather than surgery for the following reasons [8]:
In the case that Patellofemoral Pain Syndrome rehab fails, a surgical consultation is indicated.
That being said, it is recommended to complete 6-12 months of Patellofemoral Pain Syndrome rehab before pursuing a surgical consultation [9].
This section of this blog write up is dedicated to explaining how Physical Therapy can help with Patellofemoral Pain Syndrome rehab.
You will learn below how Physical Therapy can help with:
The first step in Patellofemoral Pain Syndrome rehab is first diagnosing it. If you remember how this condition is diagnosed, then you know all other injuries must be ruled out first.
Our injuries that present similar to Patellofemoral Pain Syndrome include [1] [8]:
Have you heard of all of these before?
If you haven’t, I hope you can appreciate the importance of working with a good Physical Therapist when beginning Patellofemoral Pain Syndrome rehab.
Not only is a thorough biomechanical evaluation necessary, but so is a Physical Therapist that is knowledgeable in knowing everything that must be ruled out first.
Nevertheless, a Physical Therapist can definitely help with this aspect of Patellofemoral Pain Syndrome rehab, you just need to find a good one!
There is some evidence that shows different subgroups of people may have different risk factors for developing this condition
For example, quad weakness was found to be a risk factor for the military population, but not for the adolescent population [5].
Knowing that risk factors for different subgroups of people can be different is important to know. This will influence Patellofemoral Pain Syndrome rehab decisions.
In other words, quad strengthening should be prioritized in the military population, where it may not be as important in the general adolescent population.
Are you confused, again? Me too.
Thankfully, people unlike me love conducting studies.
The conflicting evidence on BMI may be explained by a study that looked at physical activity levels in those with Patellofemoral Pain Syndrome. It was found that adults were much less active than adolescents [6].
As a result, higher BMI being a risk factor for adults, but not the younger population, may be due to the fact that adults with this condition are less physically active.
This is another example of how Patellofemoral Pain Syndrome rehab can be influenced by knowing risk factors. Even though higher BMI has not been identified as a risk factor in teens, it may be important on prioritizing a physically active lifestyle to prevent reoccurring symptoms.
In summary, you should feel that your Physical Therapist is making your Patellofemoral Pain Syndrome rehab unique to YOU!
If you don’t feel like this, go somewhere else before you get stuck thinking “it will get better eventually” and 25 visits later not much has changed.
When a teenager comes to me to begin Patellofemoral Pain Syndrome rehab, I always mention the importance of living an active lifestyle.
I know it may seem super generic when I say that, but it is true! I already touched on this, but let me remind you.
The reason behind this likely has due to the fact that adults with Patellofemoral Pain Syndrome are less active [6].
Now do you get why I mention the importance of an active lifestyle?
This is why I frequently advise patients to complete a walking program for Patellofemoral Pain Syndrome at home.
For almost every injury, there have been risk factors identified that increase one’s chance of developing a specific injury.
Furthermore, risk factors can be organized by modifiable (what can be changed) and nonmodifiable risk factors (what cannot be changed).
For example, if being older than 40 is a risk factor for developing an injury, this would be a non-modifiable risk factor as time machines are not real!
In terms of Patellofemoral Pain Syndrome, there are LOTS of modifiable risk factors that can be addressed. Some examples include [1] [5]:
Your Physical Therapist should perform a thorough biomechanical evaluation during your first visit. By doing this, your Physical Therapist will be able to identify any deficits that can be addressed that may reduce the risk of developing Patellofemoral Pain Syndrome in the future.
As this condition is complex, there are many different treatments your Physical Therapist may utilize.
Some other treatment options for Patellofemoral Pain Syndrome include:
Just because there are so many treatment options for Patellofemoral Pain Syndrome rehab, does not mean they are all beneficial! Matter of fact, some of the treatment options mentioned above should NEVER be used.

It is highly recommended that dry needling (pictured above) should not be performed for the treatment of individuals with Patellofemoral Pain Syndrome [1].
There may be a time and place to utilize some of the treatments mentioned above.
However, they should NEVER be utilized as the ONLY treatment [1]. That is, strengthening and/or running retraining should be the main focus during Patellofemoral Pain Syndrome rehab, with other treatments used sparingly.
The timeline for recovering from Patellofemoral Pain Syndrome is something that your Physical Therapist should address during your first visit.
However, you may have to take what your Physical Therapist tells you with a grain of salt.
For example, if they say, “You will be good to go in a couple months”, you may be left feeling disappointed two months later.
Let me tell you why this is.
The truth is that everyone’s recovery from this condition is different. There are so many factors that influence one’s recovery from Patellofemoral Pain Syndrome. Some examples include:
Furthermore, it is common for two people with Patellofemoral Pain Syndrome to respond differently to the same treatment.
For example, strengthening the hip abductors may help one person, but may not help someone else with Patellofemoral Pain Syndrome.
Because of this, there is some trial and error that occurs in order to find the best treatments during Patellofemoral Pain Syndrome rehab.
That being said, as long as your compliance with Patellofemoral Pain Syndrome rehab is high, it is currently advised to inform patients they will see improvements within 6-12 weeks [8].
Notice that I said “improvements” and not “full recovery.” This is because complete recovery may take much longer!
In summary, your Physical Therapist should not simply say, “You will be good to go in a couple months.” Rather, they should inform you on the following:
If you have had Patellofemoral Pain Syndrome or not, I hope you can at least appreciate how much advice a Physical Therapist can provide throughout Patellofemoral Pain Syndrome rehab. Also, you should now begin to have an expectation of what to look for in a Physical Therapist.
If you made it to this point of the blog, I haven’t even got into the good stuff yet. I am just getting started. So take your bathroom break, grab a snack, do whatever you need to do because up next: walking, strengthening, and more.
By now you should understand the importance of maintaining an active lifestyle if you are suffering from Patellofemoral Pain Syndrome.
If you don’t understand, I will give it one last attempt.
In a 2017 study, it was found that adults with Patellofemoral Pain Syndrome walk almost 3,400 less steps than healthy adults. This would result in approximately 1.2 million less steps per year [6].
Furthermore, in this same study, the authors compared how often healthy adults and adults with Patellofemoral Pain Syndrome achieved 10,000 steps a day over a 2 week period.
It was found that 75% of the healthy adults achieved the 10,000 daily steps, while only 20% of adults with Patellofemoral Pain Syndrome did [6].
If you are still rolling your eyes at me, I just hope you are rolling your eyes at me while walking!
Anyways, I often prescribe a walking program for Patellofemoral Pain Syndrome at some point during Patellofemoral Pain Syndrome rehab for the reasons mentioned above.
It is debated whether or not tight hamstrings, quadriceps, and/or gastrocnemius are risk factors for developing Patellofemoral Pain Syndrome.
Nevertheless, if restricted mobility is identified, it does not hurt to address those deficits.
Improving mobility may or may not reduce risk for developing future Patellofemoral Pain Syndrome, but it doesn’t hurt to try!
Also, improving mobility deficits can assist in preventing other injuries from occurring in the future.
There have been lots of studies performed aiming to identify the best strengthening exercises for Patellofemoral Pain Syndrome rehab [1] [7] [10] [11] [12] [13] [14].
Some common strengthening interventions that are used with Patellofemoral Pain Syndrome rehab include:
A confusion in regard to Patellofemoral Pain Syndrome rehab is knowing what the best strengthening strategy is. Check out my blog post to learn what strategy for strength training for Patellofemoral Pain Syndrome rehab is best.
Patellofemoral Pain Syndrome is common amongst individuals who run regularly. This is one reason why overuse is thought to be the main cause of this condition.
Your Physical Therapist can perform a running evaluation to assess changes that could be implemented that may decrease pain.

Some examples of what your Physical Therapist will assess during a running evaluation include [1] [3]:
If you haven’t picked up on the trend yet, let me inform you:
Nothing about Patellofemoral Pain Syndrome is straightforward
In summary, I hope you can imagine the importance of working with a Physical Therapist that is familiar with Patellofemoral Pain Syndrome rehab.
Just because this blog is written by a Physical Therapist, does not mean all are up to date with Patellofemoral Pain Syndrome rehab.
Do your research.
Ask around.
And find a good Physical Therapist!
This site uses Akismet to reduce spam. Learn how your comment data is processed.

Steve
Posted at 14:18h, 20 MarchI have read several articles on Patellofemoral Femoral Pain over the years and I have to say that this is up there with the best of them in being super thorough and informative! Looking forward to reading the rest of your articles.
Casey Ebelt
Posted at 13:52h, 21 MarchI appreciate the kind words, Steve!